Keeping Our Bones Strong As We Age
By Meredith Kimple
How many of us were encouraged to drink a glass of milk every day when we were children? The importance of strong bones is drilled into our heads from an early age, but the effects of an inadequate calcium intake are not obvious until we are much older. We all lose a significant quantity of bone mass throughout the aging process, and our bodies are no longer able to effectively absorb the calcium and vitamin D needed to maintain bone strength and density.
What factors contribute to this loss of bone mass in older adults?
A diet that is lacking in both calcium and vitamin D may leave older adults vulnerable to weak or brittle bones. As mentioned in previous blog posts, a senior’s poor diet can be the result of numerous factors, including financial constraints, the physical challenges of food preparation, or a decreased appetite. However, even if an older adult ingests the daily-recommended amounts of calcium and vitamin D, their bodies may not be able to properly absorb them; this in turn means that they require an even greater intake of vitamins and minerals than younger adults.
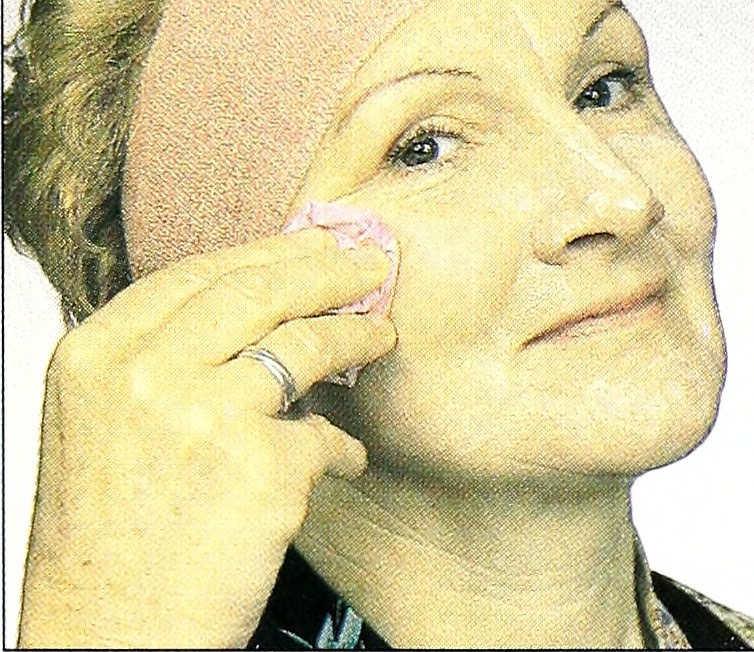
While we tend to associate bone strength with the intake of calcium, vitamin D is an equally vital part of supporting and preserving healthy bones. One of the easiest natural ways to acquire vitamin D is to spend time outdoors; our bodies absorb direct sunlight through the skin and then process it as vitamin D. Some older individuals do not receive an adequate amount of sunlight, either because they are institutionalized or confined indoors by severe mobility impairments. As with calcium, an older body has greater difficulty converting sunlight into vitamin D than a younger body.
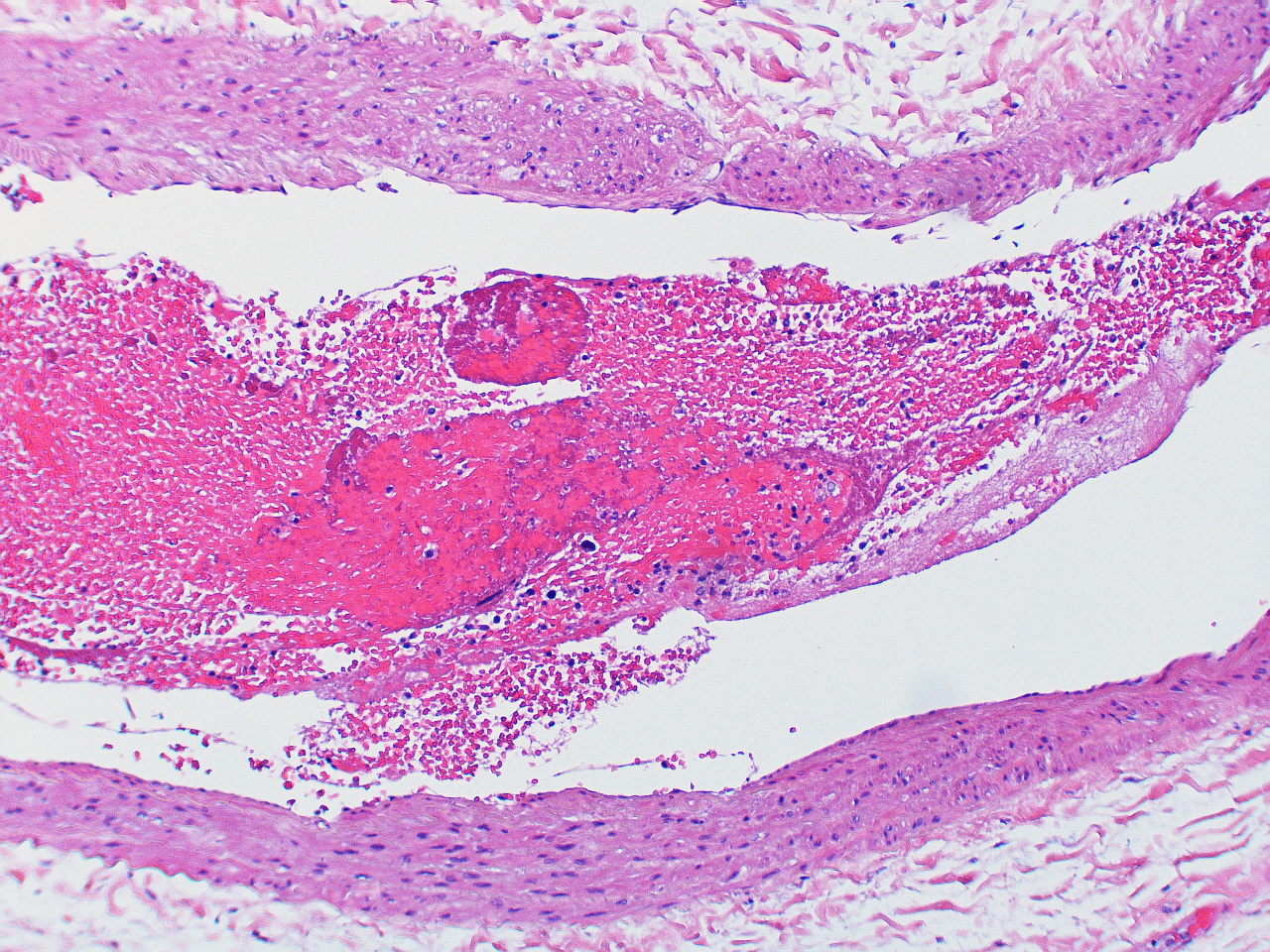
Post-menopausal women are particularly at risk for reduced bone strength, primarily due to their rapid loss of estrogen; men face a greater risk for weaker bones after they reach 70 years of age. Up until the age of 40, our bodies constantly remove and replace any lost bone mass with new bone, but as we age, this process occurs far less frequently. Certain medications can also contribute to the loss of bone mass.
You might think that having brittle or weak bones is not the worst condition a senior could face, considering the prevalence of Alzheimer’s disease, stroke, and cancer. But frail bones can lead to truly devastating accidents.
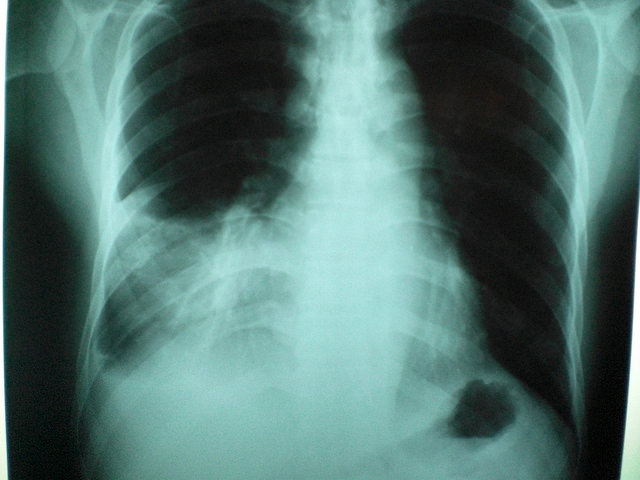
An older adult with weaker bones may be more prone to falling, which can then lead to broken bones or other serious injuries. Changes in their bone structure can cause an unsteady gait or stooped posture, both of which make walking a greater challenge and reducing mobility. And, of course, an older person may develop osteoporosis, a bone disease characterized by severe loss of bone density. An older adult with osteoporosis is more likely to break at least one bone if they fall, but their bones are so weak that even a strong sneeze or cough can cause a serious fracture.
At an advanced age, our bodies are not as well equipped to handle even the most minor fractures or broken bones. More serious injuries, like a broken hip, can subject an older individual to a debilitating surgery and long recovery, both of which may leave them susceptible to disease and decline. Brittle bones can bring an otherwise healthy older adult to the brink of frailty, and limit their ability to move without causing irreparable damage to their body.
Though the optimal time to reinforce our bones with calcium and vitamin D is prior to our 30s, there are things we can do now to help our older loved ones (and ourselves). Absorption may not be nearly as effective, but it is crucial that our loved ones are getting enough calcium in their diets; the first foods that come to mind are dairy products, like milk or yogurt, but calcium can also be found in certain vegetables, like broccoli and kale. Vitamin D deficiency is fairly common across all age groups, and our older loved ones may not be getting enough from sun exposure or their diets. Calcium and vitamin D supplements may help bolster your older loved one’s balanced diet, filling in the gaps caused by inefficient absorption; make sure they speak with their physician before adding any vitamins or supplements to their diets.
Exercise is another great way to improve and maintain bone strength. For many seniors, physical changes and limitations can mean the loss of their preferred form of exercise; strenuous activities, like running, stair-climbing, or weightlifting, may prove too difficult, taxing, or dangerous. Instead, they may benefit from gentler forms of exercise that do not wreak havoc on the joints, like short daily walks, jogging, yoga, Tai Chi, or dancing. If your older loved one cannot exercise due to mobility impairment, encourage them to see a physical therapist, who can help them adapt activities and design a unique exercise regimen that is tailored to their abilities. In addition to strengthening their bones and muscles, regular exercise can help to improve an older adult’s sense of balance, which gives them more confidence when walking.
It’s easy to believe that by the time we reach old age there is very little we can do to fortify our bones. While there is certainly no way to reverse the aging process or make up for lost time, to say that we are utterly powerless would be a gross exaggeration. If we can help our older loved ones eat better and exercise, we are helping them to make modest improvements in their health; on the other hand, if we do nothing, their bones can only grow weaker and continue to lose mass. As is the case when tackling many of the ailments that afflict the elderly, small lifestyle changes like an improved diet and regular exercise can have a positive impact on overall health and wellness.
You’re never too young or too old to be proactive in protecting the strength and health of your bones, so after you pour that glass of milk for your older loved one, make sure you pour one for yourself too!